Exciting game. High tension right up to the last minute. Will the patient survive? Will he not survive? Will the game go into extra time? No carer in the penalty area and the 30-second delay was 10 seconds too much. Emergency bronchoscopy. Get the mucus that has slipped into the lungs out again somehow. In other words, deprive the patient, who can hardly breathe anyway, of ventilation. Push the camera down the throat and into both lungs. Switch on the aspirator and suck in as much as it can. I've had it four times in my eventful life. That's enough. But I'm sure my life will go into overtime even more often. It's always gone well so far. So far. Let's hope I can avoid the penalty shoot-out for much longer. If it comes to the final for an ALS patient like me, it might be final. Maybe even wishfully. Who knows what's left of the Swiss cheese.
I live with a feeding tube. On festive days like New Year's Eve, I watch my friends and family feast. Meanwhile, fluids and nutrients trickle through a hole in my stomach at a rate of 120 ml per hour directly into my stomach. I don't notice any of it. I no longer taste anything. Except in the case of reflux, when the stomach contents go in the wrong direction. I can taste vomit.
If it runs in the right direction, it still doesn't run properly. The drain no longer works. That's why I have another hole in my stomach. A little further down. It's called Pufi. Show-offs call it SPBK. They emphasise that it stands for suprapubic bladder catheter. Particularly clever ones add at every opportunity that the difference to the non-invasive version is a catheter that is inserted into my bladder through the penis. I had that before. It sucked during sex. Spontaneous is not. Pulling is not such a problem. But after the act, the thing has to go back in somehow. And that's quite an act.
Shit is a good keyword. I don't like the laxative thing any more either. A suppository with laxative. Pushing an enema afterwards, because the suppository is rarely powerful enough. If you're not familiar with enemas, it's basically an enema. Pump liquid into the bum with a syringe so that the storm tide in the bowel pushes everything into the nappy. I recommend putting a disposable pad underneath in bed. You can get a lot out with this method. The rest can be scraped out with your finger. There is no other way to be clean. But are you too uncomfortable to ask for it? You know first-hand that some carers don't even understand their own colleagues who do this. No, I would never ask. That's why you're dirty most of your life.
But I only feel really bad when I have problems breathing. In the past, I could at least improve the feeling by breathing faster. With a breathing mask, I could fake a leak with my mouth. The ventilation then gave me air immediately. That was great. Prevented many a panic. And made many a breathing emergency more bearable. To make matters worse, I've had one more hole in my body for a few days now. I have had a tracheostomy tube inserted. For reasons. Now the air goes through a hole in my throat, almost in my chest actually, directly into my lungs. There's no more triggering, as the ventilator shock is called. I only breathe what the machine tells me to breathe. That's twelve breaths a minute for me. Every minute. Every minute. The machine doesn't care if I'm out of breath. Whether I have shortness of breath. Whether I'm panicking. It allows me twelve breaths. Minimum and maximum. My will is no longer worth anything. Neither is my sense of smell, by the way. You can't smell anything with a cannula. Nobody told me that.
I have never needed so many tranquillisers in such a blatant dosage and form of administration in my entire life to prevent me from completely freaking out. Five 1 mg Tavor injections in a row. Not the familiar tablets, but as an injection solution. Injected directly into the bloodstream. Immediate effect. Recommended maximum dose according to the manufacturer 0.5 to 2.5 mg per day. I needed five. Even though I was in the best possible environment. In the intensive care unit with really competent nurses, doctors and therapists. I also had my own carers with me. I should have felt safe.
I can only communicate with my eyes. At best, via my eye control and the voice output on my computer, which I stare at day in, day out. At least in theory. I write all this with my eyes. I'm really good at it. But when secretions run past the balloon of the cannula again, or even easier to visualise, when mucus forms in the lower airways and slides like shit into the lungs... the eye control thing doesn't work anymore. You can no longer focus your eyes on the tiny letters. It no longer works when I have trouble breathing during an inhalation because a lot of mucus has come loose again. I can't hit the keys in my excitement. I can't even type "stop".
If secretions slip into my lungs and I find myself in a life-threatening situation, nothing works with the computer. I have to be able to rely on those caring for me to understand my eye language without any restrictions. I won't be dead in five minutes. Not in two minutes, when you can revive me. Welcome to the penalty shoot-out. Not in thirty seconds, you can call a team of doctors for a bronchoscopy. Welcome to extra time.
If you want to spare me this unworthy-of-life shit, you have to be able to read my eyes. I can't expect that from a hospital employee. How could you? It doesn't happen overnight. Not even every carer in my own team can do it smoothly. But at least I'll survive. The way I put it sounds exaggerated. But I'm serious. I think back to a certain situation in the hospital, but stop the thought. Try it. Shit, damn it, think of something else. Shortness of breath. Too late. Shit.
25 minutes later.
I had to interrupt my writing. My pulse is still racing. Terrible. We coughed, aspirated, inhaled, aspirated, coughed, aspirated. Hardly any noticeable change. I'm beside myself.
My guests have finished eating. My beautiful girlfriend pours wine for everyone. My friends, my parents, herself. Well, yes. Almost everyone. I am injected with opiates. The pain from the cannula is unbearable at times, even by my standards. It wouldn't be so tragic if there was more to me. At least a bit of tissue. But there isn't. If the stitches hadn't grown in, they wouldn't have had to be surgically removed, the wound wouldn't have had to be torn open again, painful wild meat wouldn't have grown in the meantime, it would be half as bad. But it wasn't.
When we're not busy nursing pain, we vacuum, take care of the wound, vacuum, cough, vacuum again and realise that we should have laid me down an hour ago to prevent pressure sores. But you don't get anywhere here. My carer on night duty today is busy with me non-stop while my visitors are celebrating. I'm in the middle of it all and yet I'm not there. When I imagine what it would be like without my own carer who is there just for me, it's unimaginable.
I've been thinking that a lot over the past few weeks and months. IPReG and RISG send their regards. Our former Minister of Health, the esteemed Mr Spahn, introduced an inhumane bill at the time. Unsurprisingly, he was unsuccessful with it. It is very surprising that the following traffic light government is sticking to it. As if Mr Lauterbach's coronavirus policy had not gone down in history enough. After countless revisions, it is now law. Perhaps no longer as inhumane as in CDU/CSU times, but still inhumane. In short: 1:1 intensive care should disappear.
This rings all the alarm bells for those affected. I have just completed four weeks of direct comparison on my own body. Well, half of it. Correct, a third, actually.
So far, I have been living at home with 1:1 care. I always have a carer with me who has relevant experience with fully ventilated ALS patients and is there exclusively for me. That costs a lot of money. It's understandable that the Ministry of Health wants to reduce this mountain of costs. The solution is to move patients into shared flats. This is because they work with a 1:3 care ratio. That costs much less. And not everyone has to have so much experience. You can ask your colleagues. In theory, of course, everyone would be qualified. But that's not even the case in intensive care at home, where "the best of the best" carers work. Anything beyond that is unrealistic wishful thinking.
I can only imagine what that would mean for patients like me. But I now have a comparison with a really good 1:2 fitting. Due to the many construction sites of the Swiss cheese - new pufi, new tracheal cannula, ingrown toenail, massive shortness of breath every day, gastrointestinal tract running amok, deaf right ear - and the complications - ingrown sutures on the stoma and the pufi, leaking cannula and necessary change, insertion of the wrong cannula and resulting new change of cannula, diagnosed water both in the lungs and under the lungs, dysfunction of the pufi - I have just completed four weeks in intensive care. They work with a nursing ratio of 2:1. That's even more patient-friendly than what the federal government wants to do to us (3:1).
I would like to emphasise very, very clearly that I received excellent care at the Wolfratshausen district clinic. It's important for me to emphasise this so that what I'm about to say doesn't give the wrong impression. It was by far the best hospitalisation of my life. But... but... without my own 1:1 care... I might have been resuscitated at some point. Or dead.
Yes, I'm serious. My quality of life would certainly have been reduced to zero. My will to live would certainly have suffered greatly. That would certainly be reason enough to consider this type of care unlawful.
There are now sample letters that contradict the imposition of such care.
But I don't know of any pattern that conveys our situation, the situation of a person affected. It's either bureaucratese, which is correct in terms of content but has no real substance. Or they are exaggerated descriptions that border on polemics. Sometimes the statements are just as insulting to public figures as the law itself. That doesn't help us all. It doesn't help anyone.
The problem is that doctors and health insurance companies are bound by the law. And I accuse the legislators, be they Mr Lauterbach, Mr Spahn or others involved in the legislation, of ignorance. Don't be angry. It's not an affront.
Yes, of course it would be their job to deal with the issue. But nobody has ever sat next to an ALS patient for 24 hours and got an idea of what it means to be dependent on 1:1 care. Whether in hospital, at home or in a shared care home. It doesn't matter. I always need 1:1 care at all times. Even in the ambulance. And there are so fucking many serious illnesses. No two are the same. And no ALS is like any other. ALS is also a rare disease. Statistically insignificant.
How could one expect a health minister to be familiar with this and set sensible guidelines for the assumption of costs by health and care insurance funds? An affected patient would have to show what a 24-hour day can look like. An affected patient would have to show why 1:1 care is not a luxury for them, but a vital necessity. Should have, would have, would have, bicycle chain. Who should do that? I don't even have a bike.
No. I'm not resting on my laurels.
From now on, there is no excuse for ignorance. I am sure that this contribution of mine will find its way via the unfathomable paths of the internet to the ministry of our health minister.
Here they are, the 24 hours in the life of an ALS patient who spent four weeks in intensive care (2:1) and had his own carers (1:1) with him. It's not every day like this. It was by chance that I documented a day that wasn't exactly calm. But, and this is the crux of the matter, the day wasn't unusually busy either. It looks excessive even to me in retrospect. But at the end of the day, it was a day like any other for me. KbV. No special incidents. The problems with bowel movements dragged the day out a bit. I normally go to bed between two and three o'clock. But even these outliers due to poo problems happen every few days. I just wrote down, hand on heart, give or take five minutes, what happened that day. I vouch for the accuracy and truth with my life. You'll get an insight into my life that you've never had before.
To keep it as close to life as possible, I'm simply including my notes from the hospital here. Unchanged. I won't correct any typos, I won't change the technical/military time stamps into nicer readable times, I won't make a nice table out of it.
Because... well, to be honest, bear with me. It's New Year's Day, I'm writing all this with my eyes while my carer tries to finish the regular replacement of my breathing tubes. I have to keep interrupting him because I suddenly need to cough or aspirate or both or need painkillers again. While my girlfriend lies next to me in bed and fortunately works herself. Otherwise she would probably kick me out of my own flat. We don't have ten minutes together at a time because there's always something going on. And I can do without time alone. Even at night, my carer lies in the guest bed next to us. The risk of a life-threatening situation unexpectedly arising that requires immediate action is too great. No, 1:1 care is not something I wanted. It is the least of all evils in order to survive and live.
And life, at the end of the day, I do it anyway.
It's New Year's Eve, 11.39pm. My first New Year's Eve without a single drop of alcohol. I don't feel like it. I just want to breathe properly and be pain-free. I have significantly more Piritramid injected than usual, a very strong painkiller. And I'm finally pain-free and my breathing is slowly getting better. Now the party begins for me, which turns out to be one of the best New Year's Eve nights for me thanks to the most wonderful company you could wish for. And a much more well-rested New Year's morning, slash midday, than I was allowed in hospital. Every morning started with a blood gas analysis (BGA), for which they cheerfully prick your ear until it bleeds onto your pillow to determine the CO2 content in your blood...
630 BGA, suction, storage
800 Drawing up, balancing and storing medication
900 rounds, with the support of
0910 Meanwhile emergency, according to machine only 100ml breathing volume, immediate suction (here it is a matter of seconds to avert complete respiratory arrest and necessary resuscitation)
925 document
930 Bearings
940 Handover
1000 Short cat wash face
1015 Storage for discharge
1020 Administration of medication
1030 Administration of medication
1035 Preparation of tube feeds, balancing
1040 Administration per bolus
1045 Suction
1050 Coughen, suction
1055 Preparation of both inhalations
1100 Right eye problems, multiple rinses, eye drops
1115 Fetching, brewing, balancing, administering coffee
1120 Emergency coughening and suction due to sudden shortness of breath (this is a matter of seconds to avert a panic attack)
1125 Inhalation medication
1135 Suction, coughen, suction
1140 Pain attack on cannula after supraglottic suction, Dipi administered intravenously
1143 Documentation, especially since BTM
1145 Inhalation NaCl
1150 COVID test
1155 Suction, coughen, suction
1200 Clean tools, replace slimy hoses
1215 Ear drops and nose drops due to inflammation
1230 Watch out for me while the drops are working, as my head is turned to the left (no communication)
1235 Phone call with my parents about expected transport tomorrow
1245 Nose constantly running, wiped and nasal suctioned
1255 Positioning changed because ischial tuberosity hurts
1300 medications prepared, balanced and administered
1305 Tube feeding prepared, balanced
1315 again problems with eye, rinsed
1320 Interruption for blood sample due to potassium deficiency
1330 Scheduled pulling of brown needle
1335 Giving tube feed
1340 Finally got round to cleaning bowel movements
1345 interrupted for suction
1350 Determined that bowel movement is only yellow mucus, documented for doctor
1355 cleaned, second attempt
1405 Eye control has hung up
1415 Fentanyl patch changed and documented (BTM)
1420 BGA, new addition created
1435 Suction
1440 Wound care right ear
1455 Shaving first half (very time-consuming, as every little movement of the neck leads to unimaginable soreness and has to be interrupted again and again)
1520 Tube feeding prepared, balanced, administered
1530 second part shaving
1555 Sucked off twice
1605 Doctor's consultation, today's or tomorrow's discharge postponed to the day after tomorrow at the earliest
1625 Suction
1630 Duty planning (rescheduling due to postponed discharge date, two carers are required for transport)
1645 Storage, cleaned, discharge unsuccessful
1655 Oral and dental hygiene (yes, only now, just haven't had time yet)
1720 Medication prepared, mortar glued, new mortar and new medication organised
1730 Medication prepared, balanced and administered again
1740 Wound treated by newly applied pufi'(time-consuming, as still fresh wound must be treated sterilely)
1800 Espresso doppio from the cafeteria, which is now cold, brewed, balanced and served
1805 Tube feeding prepared and balanced
1806 Administration of medication i. V. from hospital
1809 Food administered
1810 interrupted for suction, too late, pillowcase changed
1820 second attempt, food administered
1825 Basic care started, moved out
1830 inhaled in the process, initially obtained medication for this (from hospital, due to prescription of strict balancing
1835 Balance sheet reconciled with hospital staff
1840 Started inhalation, fetched warm water for basic care because by now it was as icy cold as my carer's cappuccino, which was brought from the cafeteria shortly before 5pm and hasn't been touched since
1842 Acute respiratory distress, oxygen 2 litres connected
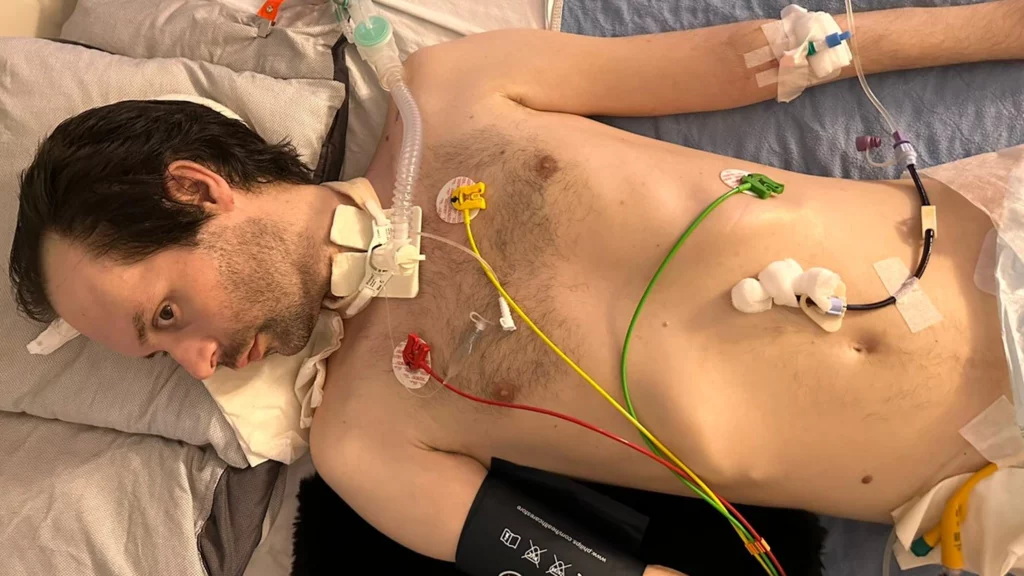
1845 Basic care of right arm, monitoring blood pressure and pulse taken (see photo)
1848 Basic breast and abdominal care (time-consuming, as ECG, PEG, Pufi, catheter; see photo)
1850 new rash/pustules on chest documented
1850 Suction, coughening, suction, shortness of breath remains
1855 Carer forced to take a breakfast break. A very unfavourable time, but visibly so exhausted that anything else would make even less sense
1905 Less than 10 minutes later, the carer cancels her meal because my breathing is becoming too unstable (especially breathing volume too low). Suction, cough, suction, excessive cough again, suction again. No significant improvement
1920 Concentrated 3% NaCl inhalation prepared and attached
1925 Basic care: left arm washed (caution required due to access; see photo)
1927 PEG mobilised, dressing change
1930 Suction, coughening, suction, moderate success, leave on oxygen
1935 Basic care: right leg, already suctioned again, right half of body positioned
1940 Wound care of operated toe
1941 interrupted due to sudden high abdominal pressure and acute breathing problems again, stored for laxation (third attempt today), laxatives organised (balancing)
1950 interrupted for coughing and aspiration due to shortness of breath
2000 next super GAU prevented by own carer, as hospital no longer has my usual laxative in stock and the alternative preparation issued is based on soya beans, to which I am known to be highly allergic (react to the smallest amounts with shortness of breath, just the right thing at that moment)
2020 as hospital cannot find another suppository, taken from own secret supply from home
2020 right eye stuck shut again, rinsed several times
2025 to 2110 Stoma care and dressing change, extensive sterile work necessary as fresh, still bleeding and suppurating wound (a level of pain that I have never experienced in 44 years of life, it is seriously beyond words). Presumably due to mobilisation, sudden accumulation of secretions in the cannula, respiratory volume drops rapidly and eye control fails at this very moment. No joke. All running applications are terminated and the computer is unintentionally restarted in the system log. The only way to communicate that I need suctioning immediately and, unusually, no coughing (because that would push everything into my lungs and make it worse) is via agreed eye control. Unthinkable with hospital staff. Due to pain after wound cleaning, strong painkiller (Dipi) requested by hospital staff and administered intravenously. After that, a short breather for both of us, which was a borderline situation even for our perfectly coordinated team. I just had a bronchoscopy the day before yesterday and can happily do without one for the next twelve months. Small talk, for the first time really today, while we wait for night duty.
2110 flowing handover "on the side", as daytime service was practically unable to document anything today
2120 Preparation of tube feeds, balancing, administration
2130 Wound care toe, dressing change
2150 Third laxative attempt also unsuccessful, cleaned, stored
2205 Suction
2210 Inhalation medication
2220 Suction, Coughen, Suction
2230 Inhalation NaCl 0.9% (standard)
2240 Suction, coughen, suction
2245 -2335 I need a break, tongue falls between my teeth after every suction, obvious exhaustion. I haven't answered any WhatsApp messages since midday today and send a standard copy & paste message to everyone. Carer tidies up and cleans work surfaces and eats something.
2335 Pause interrupted for suction
2340 Head turned to left side for application of ear drops due to inflammation, observed during exposure time for known reasons
0005 Suction
0010 0120 Pause ,
0120 Suction, head position corrected as ear hurts (oh yes, in addition to the outer ear infection I also have an open wound on the earlobe from lying down and a pressure sore below the ear (remnants of the straps of my NIV masks)
0125 Urge to urinate and spontaneous bowel movements, only yellow again
0145 Pain at wound site on neck, strong analgesic requested and administered intravenously
0155 Very liquid stools suddenly, makeshift disposable pad placed underneath at the last second
0235 Suction, bowel movement cleaned
0245 Suction, coughing, suction
0245 Preparing medication
0250 Storage for sleeping
0300 Suction, coughing, suction
0310 Administration of medication
0315 to 0330 due to unbelievably annoying rattling in my throat, coughed for a long time again, vacuumed, finally tiredness won out and I fell asleep with rattling
0330 to 0430 Carer tidies up, cleans (I noticed) and documents'(I assume the light at the table was on for so long)
0430 Storage
0600 Storage
0640 Every day the same game, nurse from the hospital comes to the daily meeting and smears my ear with Finalgon (preparation for BGA)
0705 BGA
0730 Storage
0800 Medication prepared and administered
...and another day takes its usual course.